|
|
Patient Info
|
Total Hip Replacement
Find out more about Total Hip Replacement with the following link
Introduction 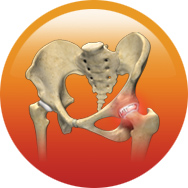
Hip replacement has become necessary for your arthritic hip: this is one of the most effective operations known and should give you many years of freedom from pain.
Once you have arthritis which has not responded to conservative treatment, you may well be a candidate for total hip replacement surgery.
Arthritis 
Arthritis is a general term covering numerous conditions where the joint surface (cartilage) wears out. The joint surface is covered by a smooth articular surface that allows pain free movement in
the joint. This surface can wear out for a number of reasons, often the definite cause is not known. When the articular cartilage wears out, the bone ends rub on one another and cause pain. There
are numerous conditions that can cause arthritis and often the exact cause is never known. In general, but not always, it affects people as they get older (Osteoarthritis).
Other causes include
- Childhood disorders e.g., dislocated hip, Perthe's disease, slipped epiphysis etc.
- Growth abnormalities of the hip (such as a shallow socket) may lead to premature arthritis
- Trauma (fracture)
- Increased stress e.g., overuse, overweight, etc.
- Avascular necrosis (loss of blood supply)
- Infection
- Connective tissue disorders
- Inactive lifestyle- e.g., Obesity, as additional weight puts extra force through your joints which can lead to arthritis over a period of time
- Inflammation e.g., Rheumatoid arthritis
In an Arthritic Hip
- The cartilage lining is thinner than normal or completely absent
- The degree of cartilage damage and inflammation varies with the type and stage of arthritis
- The capsule of the arthritic hip is swollen
- The joint space is narrowed and irregular in outline; this can be seen in an X-ray image
- Bone spurs or excessive bone can also build up around the edges of the joint
- The combinations of these factors make the arthritic hip stiff and limit activities due to pain or fatigue
Diagnosis
The diagnosis of osteoarthritis is made on history, physical examination & X-rays. There is no blood test to diagnose Osteoarthritis (wear & tear arthritis)
Indications 
THR is indicated for arthritis of the hip that has failed to respond to conservative (non-operative) treatment.
You should consider a THR when you have
- Arthritis confirmed on X-ray
- Pain not responding to analgesics or anti-inflammatories
- Limitations of activities of daily living including your leisure activities, sport or work
- Pain keeping you awake at night
- Stiffness in the hip making mobility difficult
Benefits 
Prior to surgery you will usually have tried some simple treatments such as simple analgesics, weight loss, anti-inflammatory medications, modification of your activities, walking sticks, physiotherapy.
The decision to proceed with THR surgery is a cooperative one between you, your surgeon, family and your local doctor. Benefits of surgery include
- Reduced hip pain
- Increased mobility and movement
- Correction of deformity
- Equalization of leg length (not guaranteed)
- Increased leg strength
- Improved quality of life, ability to return to normal activities
- Enables you to sleep without pain
Pre-operation

- Your surgeon will send you for routine blood tests and any other investigations required prior to your surgery
- You will asked to undertake a general medical check-up with a physician
- You should have any other medical, surgical or dental problems attended to prior to your surgery
- Make arrangements around the house prior to surgery
- Cease aspirin or anti-inflammatory medications 10 days prior to surgery as they can cause bleeding
- Cease any naturopathic or herbal medications 10 days before surgery
- Stop smoking as long as possible prior to surgery
Day of Your Surgery

- You will be admitted to hospital usually on the day of your surgery
- Further tests may be required on admission
- You will meet the nurses and answer some questions for the hospital records
- You will meet your anaesthetist, who will ask you a few questions
- You will be given hospital clothes to change into and have a shower prior to surgery
- The operation site will be shaved and cleaned
- Approximately 30 mins prior to surgery, you will be transferred to the operating theatre
Procedure

- The purpose of the total hip replacement procedure is to replace diseased worn joint cartilage with metal and plastic to reduce or eliminate pain, decrease deformity, and improve function.
- In most instances, a direct anterior approach will be used, with a small incision on the front of the hip while the patient is lying flat on their back. In some patients, a posterior approach
will be used, in which the patient is positioned to lie on their side, and a skin incision is made on the side and buttock of the hip. A deeper incision is made at the joint capsule to expose
the joint surfaces.
- The ball end of the thigh bone (ie femoral head) is cut near the base of the femoral neck and removed
- The cup socket of the hip is then reamed, and a trial cup put in place and checked for appropriate fit with digital imaging. When satisfactory position is achieved, the trial component is removed,
the socket irrigated with antibiotic solution, and a porous metal cup is secured into the hip socket with a press fit. In some instances, screws may also be used to secure the cup to the
pelvis bone.
- The choice of bearing material then determines the type of head and cup liner.
- In most instances, a polished metal liner will be secured inside the cup, and a bipolar head will impacted onto the femoral implant stem. A bipolar head is composed of a polished metal
ball pressed inside a larger plastic ball.
- The large plastic ball provides a similar function as normal cartilage
- In rare instances, depending on cost and insurance, a plastic liner and large metal ball will be used as the bearing surface instead.
- The plastic piece will slowly wear, but with the latest technological advancements, should last 20 years or more.
- The leg is then extended and rotated to exposed the top of the femur bone. The femur bone is then broached to accept a metal stem of appropriate size. The metal stem can be secured with cement
or by pressfit and bone ingrowth.In most instances, I will use implants that have a porous coating near the top to allow bone ingrowth, avoiding the potential problems with cement. Cement
fixation allows immediate fixation but can break down over years and create an abrasive which accelerates plastic wear and component loosening. Cement also adds another nonbiologic material
that bacteria can adhere to,so selective use of cemented implants will be utilized. However, bone quality and medical conditions can often require the stem to be cemented. The size of
the metal stem is selected to provide the best pressfit inside the bony femoral canal and to maintain leg length and hip geometry as close as possible to normal. During this part of the
procedure, bony spurs are also removed, and any excessive soft tissue is removed or released to allow optimum motion and eliminate deforming contractures or impingement.
- A trial stem and head are then put in place, and a manual test of stability throughout its range of motion is used to assess stability and avoidance of impingement. With optimum positioning
and size of the components, the risk of dislocation is reduced through proper soft tissue tension. Portable digital imaging or xray is then used to make sure the components are positioned
correctly.
- When satisfied, the trial stem and head are removed, and the hip is thoroughly irrigated with antibiotic solution, then the actual femoral implant is gently impacted in place to a good secure
pressfit.The head is then impacted onto the femoral stem.
- After implantation of the components, the hip is once again put in place and manually checked for stability and digital imaging is used once again to verify correct position of components.
The hip is then irrigated thoroughly with antibiotic solution, the deep soft tissues are closed, the skin closed with a watertight closure with an absorbable suture,sealed with glue,
and an impermeable waterproof antibacterial dressing applied to prevent secondary infection until the wound is healed.
- A sealed suction drain is typically used for 12 days to minimize blood collection and wound complications.
Postoperative Care and Rehabilitation

- Advancements in multimodal pain management are allowing patients to be discharged home same day as surgery with immediate walking. Typically, not further therapy is needed after discharge from
the hospital.
- A case manager will visit with you in the hospital to arrange for your home equipment needs
- Patients are walking and participating in therapy just a couple of hours after their surgery. Therapy will focus on walking with a walker, exercises to strengthen your leg muscles, and education
on how to prevent dislocations during the first few weeks after surgery.
- You will receive antibiotics, pain medications, laxatives, nausea medicine, and possibly blood thinners while in the hospital, depending on your risk factors for blood clots versus bleeding.
- You will also continue with medications at home. We will give you prescriptions for these prior to your surgery date so that they are available once you get home.
- We want you to leave the dressing in place until seen in the office at your two week followup visit. A waterproof dressing will be used to allow you to take a shower, but you are to avoid baths
or direct spray on the dressing during the time the dressing is in place.
- The first couple of weeks are a little rough, but you will be walking farther with less pain every day. By your two week postoperative appointment in the office, you can generally expect to be
close to transitioning from a walker to a cane.
- By 6 weeks postop,you can generally expect to be doing well, walking without a cane without pain and with full range of motion.
- By 3 months postop,you will generally be back to normal.
- Most patients, depending on their job duties, can be back to work by 46 weeks after surgery. Some jobs may require a longer time off.
- Most patients can resume driving when they can safely get in/out and operate a vehicle and are not impaired with pain medications.
Pain Control

- The use of multiple modalities for pain control allow comfort, immediate ambulation, and short hospital stay. By controlling the pain immediately after surgery, less pain medication is needed
in the following days because the pain pathway sensitization is delayed. The new techniques have allowed adequate pain control with only rare use of intravenous narcotics.
- Local Injection. Recent technological advancements in this area have allowed this modality to be the primary method of pain control. A long acting local anesthetic will be injected everywhere
around the hip, providing up to 72 hours of pain control.
- AntiInflammatories.Unless contraindicated, you will be given IV NSAIDs before leaving the operating room, and during your stay in the hospital. By inhibiting the inflammatory response to surgery,
the pain can be significantly reduced.
- Oral Pain Medication. For further breakthrough pain, oral narcotics will also be used.Typically, only low dose hydrocodone is needed, and will be given on a scheduled basis unless you become
nauseous or tired or confused.
- The oral and IV narcotics can cause constipation and nausea. Laxatives will be given to minimize the effects of the narcotics on the bowels, and antinausea medicine will be given at the end of
surgery and as needed thereafter.
Risks and Prevention

In general, you can expect 95-97%chance that your surgery will do well without complications. However, there is a possibility of a complication despite all of the precautions we take. We take precaution
to minimize the risk of complications, as detailed below (these are the most common complications, but there may be others):
Medical Complications
- Your unique medical conditions are best known by your primary care physician and other medical subspecialists. Prior to surgery, we will obtain labs and send you to your primary care physician
and other indicated subspecialists to evaluate your medical condition, determine the medical risks of surgery, and provide medical clearance for surgery. They will assess your risk of
cardiopulmonary or other medical complications and develop a coordinated plan for your perioperative medical management to minimize those potential risks. They will help fine tune your
medical condition in preparation for surgery.
- If your have diabetes, renal disease, rheumatic problems, pulmonary problems, or cardiovascular problems, your risk of complications is increased.
- It is important to keep your blood pressure under control during the perioperative period. If your blood pressure is too high or too low, you can have a stroke in the perioperative period.
You should take your blood pressure medications with just a sip of water on the morning of surgery.
- For diabetics, blood sugar may be managed with a sliding scale insulin protocol.
- If you take methotrexate or TNFa antagonists, you should generally stop them one cycle before surgery and not restart them until after the wound is healed at the first postoperative visit
to facilitate bone and soft tissue healing.
- Cardiac complications can occur despite preoperative evaluation and clearance, including myocardial infarction, congestive heart failure, arrhythmia, and even death. A cardiologist evaluation
and perioperative management will be used as indicated.
- Constipation or bowel immobility can develop after surgery and will be treated with laxatives and other means as needed.
- Urinary retention is common after surgery, particularly in elderly men. In most instances, retention is minimized with early ambulation, and on occasion, with medication. In rare instances,
a urinary catheter may be placed for a few hours.In some instances, it may have to stay in place longer
Anesthesia Complications
- Aspiration Pneumonia. To prevent aspiration of your stomach contents, please do not eat or drink anything other than your blood pressure medicines and a sip of water after midnight before
surgery.
- Atelectasis. When you undergo general anesthesia, a machine will breath for you, inflating your lungs. When that inflation pressure is removed after surgery, a small amount of inflammation
and fluid can collect in the small sacs in the lungs. It is important to drive that fluid away by breathing deeply every hour to avoid pneumonia and reduce postoperative fever. You will
be given an incentive spirometer while in the hospital to help with the deep breathing, and we will use oxygen and breathing treatments if needed.
- Your anesthesiologist will do a thorough evaluation of your medical condition and plan for your anesthesia requirements during your preoperative registration visit at the hospital, and review
that once again on the day of surgery. They can explain the options, recommendations, procedures, and risks in more detail.
Infection
- Infection is a very serious problem that is taken seriously. The implants we place can get infected at the time of surgery or at any time after surgery from bloodborn bacteria from dental
procedures, urinary tract infections, etc. If they get infected, it is often necessary to remove the components to treat the infection, and later reimplantation after the infection is
cured. This is a disastrous condition which we want to avoid and take every precaution to try to prevent.
- Your teeth and mouth can be a source of infection at the time of surgery and at any time thereafter. We will evaluate your dental health and refer you to your dentist for any concerning dental
issues and clearance prior to surgery if needed. Any dental issues must be resolved prior to a joint replacement, and surgery may be canceled if not resolved to our satisfaction. At any
time after your joint replacement, it is important to take antibiotics prior to and following any dental procedures. If your dentist cannot provide prophylactic antibiotics, ask our office
and we will prescribe them for you.
- Your nose can also be a source of bacteria that can cause infection. We will culture your nose and determine if difficult bacteria are present. We will also prescribe mupirocin antibiotic
ointment which you will use 5 days prior to surgeryto eradicate any nasal bacteria, particularly MSSA and MRSA.
- Your skin can carry a multitude of bacteria, including difficult to treat MRSA strains. You will be instructed to take a whole body bath or shower with Hibiclens antibacterial soap for 5
days prior to surgery, including the morning of surgery.
- You will also be prepped upon arrival at the hospital on the day of surgery with Hibiclens. You will also be prepped again in the operating room and a sealant iodine barrier used to wrap
around the operative site.
- Contamination during surgery can occur, but its risks are minimized by the use of clean “spacesuit” hoods, meticulous sterile technique, antibiotic irrigation, and IV antibiotics before,
during, and after surgery for 24 hours.
- Secondary infection from a draining wound after surgery can also occur. To minimize this risk, we use a watertight suture closure on the skin and apply an impermeable dressing while in the
operating room. That dressing provides a barrier to secondary infection and will stay in place until removed in our office at your 2 week followup appointment. We may also prescribe an
oral antibiotic at the time of your preop visit to be taken at home after surgery.
- If you have an active urinary tract infection, it must be treated prior to surgery. We will collect a urine sample in our lab in preparation for surgery and treat accordingly.
- Steroids delay wound healing. We prefer that oral steroids be stopped or reduced below 7.5mg/day to avoid wound complications.
- Methotrexate and other rheumatological medications also delay healing and can lead to increased risk of secondary infection or immunosuppression of your own body’s defense mechanism. Your
should stop methotrexate preferably 7 days before surgery, and not restart until 2 weeks after surgery. Other medications such as TNFa antagonists and SERMS should also be stopped at
least one cycle prior to surgery.
Blood Clots (DVT) and Pulmonary Embolism
- With reduced mobility after a joint replacement, you are at risk of developing a blood clot in your legs. If blood clots form in the deep veins of the legs (DVT), they can dislodge and travel
to the lungs where they can cause a serious and possibly deadly condition called a pulmonary embolism. Therefore, it is very important to try to prevent a blood clot from forming.
- If you have had a DVT before, you are at increased risk of having one develop again, and we may recommend a filter be placed in your main vein to catch any clots before they reach your lungs.
- The best way to prevent a blood clot is to have you walk as quickly as possible after surgery, using the normal muscular pumping motion of your body to increase the flow in the veins. We
will have physical therapy begin to work with you on the day of surgery to get you walking as quickly as possible.
- You will be instructed to also perform active motion exercises hourly while in bed, including toe curls, ankle pumps, and bending and straightening the knee. These motions simulate walking
motion of the muscles, but without the weight.
- We will also implement passive means to help with blood clot prevention, including sequential compression devices, TED hose, and usually blood thinners.
- SCDs (sequential compression devices) are attached to the calves, and a pneumatic pump inflates them to create a pressure gradient and flow in the veins of your legs, preventing blood stagnation
until you are fully mobile and able to walk. You will have these on while in bed during your hospital stay.
- TED hose are compression stockings which help compress the legs and minimize the amount of blood that can pool in the veins of the legs. We will apply TED hose or a compression dressing during
surgery, and you will wear them for 6 weeks after surgery.
- Unless contraindicated, we will use some form of blood thinners after surgery. For those at risk of bleeding, low dose aspirin 81mg will be used for 6 weeks after surgery. Please make sure
you have aspirin available at home prior to surgery so that you can take it after surgery. If you already take coumadin prior to surgery, we will resume your coumadin after surgery. For
those who are not at risk for bleeding or who are not already on coumadin, we will give Lovenox injections or an oral medicine called Xarelto. We will give these medications to you while
in the hospital, and give you a prescription for home use during your preop visit. After completion of 10 days of blood thinner, we will have you take 81mg of aspirin each day for an
additional month.
Bleeding/Blood Loss
- You will lose blood during and after surgery which may require a blood transfusion based on your clinical symptoms. With the techniques and medications that are used, transfusion is rarely
needed.
- We usually place a drain during surgery to collect blood and minimize risk of forming a hematoma. The drain will typically be discontinued on the first or second day after surgery. You may
be discharged home with the drain, and if so, it will be pulled by the outpatient therapist or home health therapist on the second day after surgery.
- During surgery, we will lower your blood pressure (ie hypotensive anesthesia) to a minimize bleeding.
- We use electrocautery during surgery to coagulate small vessels to minimize blood loss.
- During surgery we also use a local injection that contains epinephrine to constrict small vessels and minimize blood loss.
- Unless contraindicated, you will be given a dose at the start of surgery and at the end of surgery of a medicine (tranexamic acid) which will help reduce bleeding.
- We will have you discontinue aspirin, Plavix or like drugs, coumadin, NSAIDS, and any other medication that can thin your blood 57 days prior to surgery. These will be resumed after surgery
based on our directions.
- We will check your blood level prior to surgery to see if you are anemic. If you are, we may start you on a medication called Procrit to improve your anemia prior to surgery.
- Although not typically needed, an optional predonation of blood by the patient a few weeks prior to surgery allows their own blood to be given back after surgery.During the period between
predonation and surgery, the patients body can generally build back up the normal blood volume, allowing the predonated blood to replace the blood lost during and after surgery.
Contracture/Stiffness
- Your hip may have restricted motion prior to surgery.
- We will perform releases during surgery and obtain full range of motion, but it takes aggressive active rehabilitation (see above) on the patients part to maintain that motion after surgery.
Some patients make excessive scar after surgery which can lead to stiffness or contracture after surgery.
Heterotopic Ossification
- Some patients form excessive bone around the hip, which can lead to stiffness and pain.
Nerve Injury
- Although nerves are typically never lacerated, they may occasionally be stretched during surgery due to stiffness or correction of deformities. In most instances, a nerve injury is temporary
and may require extended therapy or possible bracing until the nerve recovers.
- With the anterior approach to the hip, the lateral femoral cutaneous nerve is prone to stretch injury, which can cause numbness and/or pain on the front of the thigh.If injured, most patients
recover within a few weeks to months.
- The femoral nerve is also at risk of injury in the anterior approach with compression against fascial structures during surgery. If injured, it can cause numbness and weakness in the leg
that usually recovers fully or nearly fully over weeks to months.
Fracture
- Patients with weak bone (osteoporosis) are at increased risk of fracture during the perioperative period. If a fracture occurs, it will be treated appropriately and may require additional
procedures or delay in rehabilitation.
Vascular Injury
- Very low risk, but has been reported in the literature.
Loosening or Mechanical Failure
- The implant can fail to have complete bone ingrowth into the porous coating, particularly in patients who take certain medications, have adverse medical conditions, have metal allergies,
or have reduced bone formation from any cause.
- Cemented implants can also loosen with time.
- Although rare with modern technological components, implants can fail.
- In some instances, the hip may become unstable with progressive pain and loosening, requiring the joint to be revised. This can occur with weak bone and implant migration, plastic
component wear, or soft tissue relaxation.
Dislocation
- Recent technological advancements have allowed much bigger heads to be used, which significantly reduces dislocation risk.
- With optimum positioning and size of the components, the risk of dislocation is reduced through proper soft tissue tension. A manual test of stability throughout its range of motion
is used to assess stability and avoidance of impingement. Digital imaging is used during surgery to make sure the components are positioned correctly.
- Dislocation risk is significantly increased with revision hip surgery.
- Most patients can resume near normal functions after anterior hip replacement due to its decreased risk of dislocation compared to the posterior approach. However, you will be instructed
to follow the standard hip precautions for the first few weeks after surgery until the soft tissues can heal to provide additional stability.
Continued Pain
- Although the purpose of the procedure is to reduce or eliminate pain, in some rare cases, chronic pain of unknown etiology can continue and may require the joint to be revised.
Postoperative Fractures and Injuries
- Falls or other trauma can cause fractures, tendon ruptures, or ligament ruptures. These can be minimized by using the ambulatory aids such as walkers and canes until your therapist
feels you are safe without them.
Implant Choices
The main choices for a hip implant are bearing material and type of fixation.
 Bearing Material:
. The traditional metal on plastic bearing is also an excellent choice for many patients. In the metal on plastic bearing, the spherical shaped head moves inside a plastic spherical shell liner that
is fixed inside a metal acetabular cup. Technological advancements to improve the life and wear characteristics of the plastic bearing have made dislocations and wear exceptionally rare. Recently,
a unique bearing design was introduced by Stryker Orthopedics, utilizing two metal on plastic surfaces to provide more natural motion and less wear. The modular dual mobility bearing uses a smaller metal head that moves inside a large plastic head that moves inside a fixed metal acetabular cup. Bearing Material:
. The traditional metal on plastic bearing is also an excellent choice for many patients. In the metal on plastic bearing, the spherical shaped head moves inside a plastic spherical shell liner that
is fixed inside a metal acetabular cup. Technological advancements to improve the life and wear characteristics of the plastic bearing have made dislocations and wear exceptionally rare. Recently,
a unique bearing design was introduced by Stryker Orthopedics, utilizing two metal on plastic surfaces to provide more natural motion and less wear. The modular dual mobility bearing uses a smaller metal head that moves inside a large plastic head that moves inside a fixed metal acetabular cup.
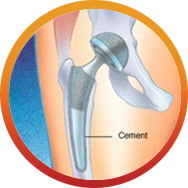 Fixation: All metal acetabular
cups are fixed with a press-fit into the bony socket of the pelvis, and sometimes reinforced with screws. Fixation of the metal stem into the femur can be by cement or pressfit. Technological advances in cement materials and techniques make cement fixation of the stem the standard for elderly patients. Fixation: All metal acetabular
cups are fixed with a press-fit into the bony socket of the pelvis, and sometimes reinforced with screws. Fixation of the metal stem into the femur can be by cement or pressfit. Technological advances in cement materials and techniques make cement fixation of the stem the standard for elderly patients.
Younger patients and patients with healthy bone are often candidates for a press-fit stem. Many of the newer press-fit stems have a porous metal coating similar to the
pores in bone to allow faster bone ingrowth.
Summary
Surgery is not a pleasant prospect for anyone, but for some people with arthritis, it could mean the difference between leading a normal life or putting up with a debilitating condition. Surgery can be regarded
as part of your treatment plan- it may help to restore function to your damaged joints as well as relieve pain.
|
|
|