|
|
Patient Info
|
Total Knee Replacement
Find out more about Total Knee Replacement with the following link
Introduction
A Total Knee Replacement (TKR) or Total Knee Arthroplasty is a surgery that replaces an arthritic knee joint with artificial metal or plastic replacement parts called the ‘prostheses'.
The procedure is usually recommended for older patients who suffer from pain and loss of function from arthritis and have failed results from other conservative methods of therapy.
The typical knee replacement replaces the ends of the femur (thigh bone) and tibia (shin bone) with plastic inserted between them and usually the patella (knee cap).
Arthritis
Other causes include

- Trauma (fracture)
- Increased stress e.g., overuse, overweight, etc.
- Infection
- Connective tissue disorders
- Inactive lifestyle e.g., Obesity, as additional weight puts extra force through your joints which can lead to arthritis over a period of time
- Inflammation e.g., Rheumatoid arthritis
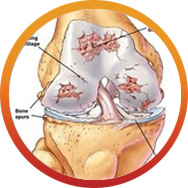
In an Arthritic Knee
- The cartilage lining is thinner than normal or completely absent. The degree of cartilage damage and inflammation varies with the type and stage of arthritis.
- The capsule of the arthritic knee is swollen
- The joint space is narrowed and irregular in outline; this can be seen in an X-ray image.
- Bone spurs or excessive bone can also build up around the edges of the joint
The combinations of these factors make the arthritic knee stiff and limit activities due to pain or fatigue.
Diagnosis
The diagnosis of osteoarthritis is made on history, physical examination & X-rays.
There is no blood test to diagnose Osteoarthritis (wear & tear arthritis).
Benefits 
The decision to proceed with TKR surgery is a cooperative one between you, your surgeon, family and your local doctor.
The benefits following surgery are relief of symptoms of arthritis. These include
- Severe pain that limits your everyday activities including walking, shopping, visiting friends, getting in and out of chair, gardening, etc.
- Pain waking you at night
- Deformity- either bowleg or knock knees
- Stiffness
Prior to surgery you will usually have tried some conservative treatments such as simple analgesics, weight loss, anti-inflammatory medications, modification of your activities, canes, or physical therapy.
Once these have failed it is time to consider surgery. Most patients who have TKR are between 60 to 80 years, but each patient is assessed individually and patients as young as 20 or old as 90 are occasionally
operated on with good results.
Pre-Operation

- Your surgeon will send you for routine blood tests and any other investigations required prior to your surgery
- You will be asked to undertake a general medical check-up with a physician
- You should have any other medical, surgical or dental problems attended to prior to your surgery
- Make arrangements for help around the house prior to surgery
- Cease aspirin or anti-inflammatory medications 10 days prior to surgery as they can cause bleeding
- Cease any naturopathic or herbal medications 10 days before surgery
- Stop smoking as long as possible prior to surgery
Day of Your Surgery

- You will be admitted to the hospital, usually on the day of your surgery
- Further tests may be required on admission
- You will meet the nurses and answer some questions for the hospital records
- You will meet your Anesthetist, who will ask you a few questions
- You will be given hospital clothes to change into and have a shower prior to surgery
- The operation site will be shaved and cleaned
- Approximately 30 minutes prior to surgery
- You will betransferred to the operating room
Procedure

- The purpose of the total knee replacement procedure is to replace diseased worn joint cartilage with metal and plastic to reduce or eliminate pain, decrease deformity, and improve function.
- An incision is made along the front of the knee, and a deeper incision around the kneecap is made to expose the joint surfaces.
- The ends of the bones of the the knee and the underneath surface of the kneecap are cut and shaped to accept metal caps which act as the part of the new joint surface. During this part of the procedure,
bony spurs are also removed, and any excessive soft tissue is removed or released to allow optimum motion and eliminate deforming contractures. I routinely remove both cruciate ligaments to enable
optimum joint balancing and minimize contractures.
- The metal pieces on the ends of the bones and underneath side of the kneecap can be secured with cement or by a pressfit with later bone ingrowth. In most instances, I will use metal components with
a porous coating to allow bone ingrowth unless the patient has a medical condition (severe osteoporosis, rheumatic disease) or takes medication which would slow bone formation. Implant cost and
a patients’ insurance plan can also impact the selection of cemented or uncemented implants. Cement fixation allows immediate fixation but can break down over years and create an abrasive which
accelerates plastic wear and component loosening. Cement also adds another nonbiologic material that bacteria can adhere to, so selective use of cemented implants will be utilized. The sizes
of the metal pieces are selected to provide the most coverage over ends of the bone without overhang.
- A plastic piece made of crosslinked high density polyethylene is then snapped in place on the tibial metal tray to act as a spacer and provide a similar function as normal cartilage. The plastic
will slowly wear, but with the latest technological advancements, should last 20 years or more.
- With optimum alignment along the mechanical axis of the leg (ie a straight line from the hip through the knee and to the ankle), the forces can be balanced on both sides of the knee, providing minimal
polyethylene wear. A computerized digital xray machine is used during surgery to make sure the mechanical axis is correct.
- Balancing the gap and ligament tension between the metal pieces is also important for joint stability and wear optimization. During the procedure, techniques are used to make sure the gap on the
inside and outside of the knee are the same, and to provide proper ligament tension to maintain the gap, alignment, and stability of the knee throughout its range of motion. Balancing the knee
is optimized by removal of the cruciate ligaments, with their function substituted with a special type of polyethylene spacer. We will also make sure that the knee can be fully straightened and
eliminate any preexisting contractures during the procedure.
- The kneecap component will be chosen to provide maximum bone coverage and good tracking throughout knee range of motion.
- Prior to implantation of the components, the knee is thoroughly irrigated with antibiotic solution.
- After implantation of the components, the knee is once again irrigated with antibiotic solution, the deep soft tissues are closed, the skin is closed with watertight absorbable sutures, the wound
is sealed with glue, and an impermeable waterproof antibacterial dressing applied to prevent secondary infection until the wound is healed. A sealed suction drain is typically used for 12 days
to prevent blood collection and swelling in the knee that can slow rehabilitation.
Postoperative Care and Rehabilitation

- Advancements in multimodal pain management are allowing patients to be discharged home same day as surgery with immediate walking. Outpatient therapy or home health is started on post operative day
1.
- A case manager will visit with you in the hospital to arrange for your home equipment needs and facilitate your continued rehabilitation needs with either home health or outpatient physical therapy.
- Patients are walking and participating in therapy just a couple of hours after their surgery. Therapy will focus on walking with a walker, exercises to maintain and improve the motion in your knee,
and exercises to strengthen your leg muscles.
- It is important that you actively use your muscles to bend and straighten your knees while in bed to avoid development of a contracture. You will also be instructed to pump your ankles to exercise
your calf muscles. We will place a pillow under your heal to help your knee be straight when resting.
- You will receive antibiotics, pain medications, laxatives, nausea medicine, and possibly blood thinners while in the hospital, depending on your risk factors.
- You will also continue with medications at home. We will give you prescriptions for these prior to your surgery date so that they are available once you get home.
- We will arrange outpatient physical therapy at a facility near your home 3 times a week (or whatever your insurance allows) for the first two weeks, then 2 times a week for another 2 weeks. If you
do not live close to an outpatient therapy center or have difficulty arranging transportation to one, we will arrange home health to provide therapy at your home.
- We want you to leave the dressing in place until seen in the office at your two week followup visit. A waterproof dressing will be used to allow you to take a shower, but you are to avoid baths or
direct spray on the dressing during the time the dressing is in place.
- The first couple of weeks are a little rough, but you will be walking farther with less pain every day. By your two week postoperative appointment in the office, you can generally expect to be close
to transitioning from a walker to a cane.
- By 6 weeks postop, you can generally expect to be doing well, walking without a cane without pain and with full range of motion.
- By 3 months postop,you will generally be back to normal.
- Most patients, depending on their job duties, can be back to work by 46 weeks after surgery. Some jobs may require a longer time off.
- Most patients can resume driving when they can safely get in/out and operate a vehicle and are not impaired with pain medications.
Pain Control

- The use of multiple modalities for pain control allow comfort, immediate ambulation, and short hospital stay. By controlling the pain immediately after surgery, less pain medication is needed in
the following days because the pain pathway sensitization is delayed. The new techniques have allowed adequate pain control with only rare use of intravenous narcotics.
- Local Injection. Recent technological advancements in this area have allowed this modality to be the primary method of pain control. A long acting local anesthetic will be injected everywhere around
the knee, providing up to 72 hours of pain control.
- AntiInflammatories. Unless contraindicated, you will be given IV NSAIDs before leaving the operating room, and during your stay in the hospital. By inhibiting the inflammatory response to surgery,
the pain can be significantly reduced.
- Oral Pain Medication. For further breakthrough pain, oral narcotics will also be used. Typically, only low dose hydrocodone is needed, and will be given on a scheduled basis unless you become nauseous
or tired or confused.
- The oral and IV narcotics can cause constipation and nausea. Laxatives will be given to minimize the effects of the narcotics on the bowels, and antinausea medicine will be given at the end of surgery
and as needed thereafter.
Risks and Prevention

- In general, you can expect 95-97% chance that your surgery will do well without complications. However, there is a possibility of a complication despite all of the precautions we take. We take precaution
to minimize the risk of complications, as detailed below (these are the most common complications, but there may be others):
- Medical Complications
- Your unique medical conditions are best known by your primary care physician and other medical subspecialists. Prior to surgery, we will obtain labs and send you to your primary care physician
and other indicated subspecialists to evaluate your medical condition, determine the medical risks of surgery, and provide medical clearance for surgery. They will assess your risk of
cardiopulmonary or other medical complications and develop a coordinated plan for your perioperative medical management to minimize those potential risks. They will help fine tune your
medical condition in preparation for surgery.
- If your have diabetes, renal disease, rheumatic problems, pulmonary problems, or cardiovascular problems, your risk of complications is increased.
- It is important to keep your blood pressure under control during the perioperative period. If your blood pressure is too high or too low, you can have a stroke in the perioperative period.
You should take your blood pressure medications with just a sip of water on the morning of surgery.
- For diabetics, blood sugar may be managed with a sliding scale insulin protocol.
- If you take methotrexate or TNFa antagonists, you should generally stop them one cycle before surgery and not restart them until after the wound is healed at the first postoperative visit
to facilitate bone and soft tissue healing.
- Cardiac complications can occur despite preoperative evaluation and clearance, including myocardial infarction, congestive heart failure, arrhythmia, and even death. A cardiologist evaluation
and perioperative management will be used as indicated.
- Constipation or bowel immobility can develop after surgery and will be treated with laxatives and other means as needed.
- Urinary retention is common after surgery, particularly in elderly men. In most instances, retention is minimized with early ambulation, and on occasion, with medication. In rare instances,
a urinary catheter may be placed for a few hours. In some instances, it may have to stay in place longer.
- Anesthesia Complications
- Aspiration Pneumonia. To prevent aspiration of your stomach contents, please do not eat or drink anything other than your blood pressure medicines and a sip of water after midnight before
surgery.
- Atelectasis. When you undergo general anesthesia, a machine will breath for you, inflating your lungs. When that inflation pressure is removed after surgery, a small amount of inflammation
and fluid can collect in the small sacs in the lungs. It is important to drive that fluid away by breathing deeply every hour to avoid pneumonia and reduce postoperative fever. You will
be given an incentive spirometer while in the hospital to help with the deep breathing, and we will use oxygen and breathing treatments if needed.
- Your anesthesiologist will do a thorough evaluation of your medical condition and plan for your anesthesia requirements during your preoperative registration visit at the hospital, and review
that once again on the day of surgery. They can explainb the options, recommendations, procedures, and risks in more detail.
- Infection
- Infection is a very serious problem that is taken seriously. The implants we place can get infected at the time of surgery or at any time after surgery from bloodbornbacteria from dental
procedures, urinary tract infections, etc. If they get infected, it is often necessary to remove the components to treat the infection, and later reimplantation after the infection is
cured. This is a disastrous condition which we want to avoid and take every precaution to try to prevent.
- Your teeth and mouth can be a source of infection at the time of surgery and at any time thereafter. We will evaluate your dental health and refer you to your dentist for any concerning dental
issues and clearance prior to surgery if needed. Any dental issues must be resolved prior to a joint replacement, and surgery may be canceled if not resolved to our satisfaction. At any
time after your joint replacement, it is important to take antibiotics prior to and following any dental procedures. If your dentist cannot provide prophylactic antibiotics, ask our office
and we will prescribe them for you.
- Your nose can also be a source of bacteria that can cause infection. We will culture your nose and determine if difficult bacteria are present. We will also prescribe mupirocin antibiotic
ointment which you will use 5 days prior to surgery to eradicate any nasal bacteria, particularly MSSA and MRSA.
- Your skin can carry a multitude of bacteria, including difficult to treat MRSA strains. You will be instructed to take a whole body bath or shower with Hibiclens antibacterial soap for 5
days prior to surgery, including the morning of surgery. You will also be prepped upon arrival at the hospital on the day of surgery with Hibiclens. You will also be prepped again in
the operating room and a sealant iodine barrier used to wrap around the operative site.
- Contamination during surgery can occur, but its risks are minimized by the use of clean “spacesuit” hoods, meticulous sterile technique, antibiotic irrigation, and IV antibiotics before,
during, and after surgery for 24 hours.
- Secondary infection from a draining wound after surgery can also occur. To minimize this risk, we use a watertight suture closure on the skin and apply an impermeable dressing while in the
operating room. That dressing provides a barrier to secondary infection and will stay in place until removed in our office at your 2 week followup appointment. We may also prescribe an
oral antibiotic at the time of your preop visit to be taken at home after surgery.
- If you have an active urinary tract infection, it must be treated prior to surgery. We will collect a urine sample in our lab in preparation for surgery and treat accordingly.
- Steroids delay wound healing. We prefer that oral steroids be stopped or reduced below 7.5mg/day to avoid wound complications.
- Methotrexate and other rheumatological medications also delay healing and can lead to increased risk of secondary infection or immunosuppression of your own body’s defense mechanism. Your
should stop methotrexate preferably 7 days before surgery, and not restart until 2 weeks after surgery. Other medications such as TNFa antagonists and SERMS should also be stopped at
least one cycle prior to surgery.
- Blood Clots (DVT) and Pulmonary Embolism
- With reduced mobility after a joint replacement, you are at risk of developing a blood clot in your legs. If blood clots form in the deep veins of the legs (DVT),they can dislodge and travel
to the lungs where they can cause a serious and possibly deadly condition called a pulmonary embolism. Therefore, it is very important to try to prevent a blood clot from forming.
- If you have had a DVT before, you are at increased risk of having one develop again, and we may recommend a filter be placed in your main vein to catch any clots before they reach your lungs.
- The best way to prevent a blood clot is to have you walk as quickly as possible after surgery, using the normal muscular pumping motion of your body to increase the flow in the veins. We
will have physical therapy begin to work with you on the day of surgery to get you walking as quickly as possible.
- You will be instructed to also perform active motion exercises hourly while in bed, including toe curls, ankle pumps, and bending and straightening the knee. These motions simulate walking
motion of the muscles, but without the weight.
- We will also implement passive means to help with blood clot prevention, including sequential compression devices, TED hose, and possibly blood thinners.
- SCDs (sequential compression devices) are attached to the calves, and a pneumatic pump inflates them to create a pressure gradient and flow in the veins of your legs, preventing blood stagnation
until you are fully mobile and able to walk. You will have these on while in bed during your hospital stay.
- TED hose are compression stockings which help compress the legs and minimize the amount of blood that can pool in the veins of the legs. We will apply TED hose or a compression dressing during
surgery, and you will wear them for 6 weeks after surgery.
- Unless contraindicated, we will use some form of blood thinners after surgery. In most instances, low dose aspirin 81mg will be used for 6 weeks after surgery. Please make sure you have aspirin
available at home prior to surgery so that you can take it after surgery. If you already take coumadin prior to surgery, we will resume your coumadin after surgery. For those at high
risk of blood clots who are not already on coumadin, we will give Lovenox injections or an oral medicine called Xarelto. We will give these medications to you while in the hospital, and
give you a prescription for home use during your preop visit. After completion of 10 days of blood thinner, we will have you take 81mg of aspirin each day for an additional month.
- We do not use a tourniquet during surgery to allow blood to continue to flow throughout the procedure, reducing the risk of stagnant blood in the veins that can cause a blood clot.
- Bleeding/Blood Loss
- You will lose blood during and after surgery which may require a blood transfusion based on your clinical symptoms. With the techniques and medications that are used transfusion is rarely
needed.
- We usually place a drain during surgery to collect blood and minimize risk of forming a hematoma. The drain will typically be discontinued on the first or second day after surgery. You may
be discharged home with the drain, and if so, it will be pulled by the outpatient therapist or home health therapist on the second day after surgery.
- We do not use a tourniquet during surgery for knee replacements, and studies have shown that the overall blood loss and need for transfusion is the same as with a tourniquet. During surgery,
we will lower your blood pressure (ie hypotensive anesthesia) to a minimize bleeding.
- We use electrocautery during surgery to coagulate small vessels to minimize bloo loss.
- During surgery we also use a local injection that contains epinephrine to constrict small vessels and minimize blood loss.
- Unless contraindicated, you will be given a dose at the start of surgery and at the end of surgery of a medicine (tranexamic acid) which will help reduce bleeding.
- We will have you discontinue aspirin, Plavix or like drugs, coumadin, NSAIDS, and any other medication that can thin your blood 57 days prior to surgery. These will be resumed after surgery
based on our directions.
- We will check your blood level prior to surgery to see if you are anemic. If you are, we may start you on a medication called Procrit to improve your anemia prior to surgery.
- Although not typically needed, an optional predonation of blood by the patient a few weeks prior to surgery allows their own blood to be given back after surgery. During the period between
predonation and surgery, the patients body can generally build back up the normal blood volume, allowing the predonated blood to replace the blood lost during and after surgery.
- Contracture/Stiffness
- Your knee may have a contracture (ie can’t completely straighten the knee) prior to surgery. If so, you will be prone to develop a contracture again after surgery.
- We will remove the contracture during surgery and obtain full range of motion, but it takes aggressive active rehabilitation (see above) on the patients part to prevent the contracture or
stiffness after surgery. Prolonged therapy or additional procedures may be needed, and in some rare cases, permanent contractures may develop after surgery.
- Some patients make excessive scar after surgery which can lead to stiffness or contracture after surgery.
- Nerve Injury
- Although nerves are typically never lacerated, they may occasionally be stretched during surgery due to stiffness or correction of deformities. In most instances, a nerve injury is temporary
and may require bracing until the nerve recovers.
- The skin incision will cut some small sensory nerves that cross in front of the knee, and a small area of numbness will be permanent on the outside of the knee.
- Fracture
- Patients with weak bone (osteoporosis) are at increased risk of fracture during the perioperative period. If a fracture occurs, it will be treated appropriately and may require additional
procedures at the time of surgery or later.
- Vascular Injury
- Very low risk, but has been reported in the literature.
- Loosening or Mechanical Failure
- The implant can fail to have complete bone ingrowth into the porous coating, particularly in patients who take certain medications, have adverse medical conditions, have metal allergies,
or have reduced bone formation from any cause.
- Cemented implants can also loosen with time.
- Although rare with modern technological components, implants can fail.
- In some instances, the knee may become unstable with progressive pain and loosening, requiring the joint to be revised. This can occur with weak bone and implant migration, plastic component
wear, or progressive stretching and relaxation of ligaments.
- Continued Pain
- Although the purpose of the procedure is to reduce or eliminate pain, in some rare cases, chronic pain of unknown etiology can continue and may require the joint to be revised.
- Postoperative Fractures and Injuries
- Falls or other trauma can cause fractures, tendon ruptures, or ligament ruptures. These can be minimized by using the ambulatory aids such as walkers and canes until your therapist feels
you are safe without them.
Implant Choices
 The main choices for a knee implant are bearing type and
fixation. The knee is not simply a hinge, but a complex joint requiring bending and rotation in addition to the absorption of impact forces. The increased wear characteristics of the motions and mechanics
make knee replacement choices slightly different than hip replacement. The main choices for a knee implant are bearing type and
fixation. The knee is not simply a hinge, but a complex joint requiring bending and rotation in addition to the absorption of impact forces. The increased wear characteristics of the motions and mechanics
make knee replacement choices slightly different than hip replacement.
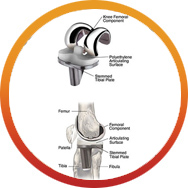 Bearing Type: All knee replacements
have a similar bearing material, a hardened polished metal femoral component moving against a plastic polyethylene insert attached to the tibia with a metal supporting tray underneath it. A plastic button
is fixed to the underneath side of the patella to provide an additional bearing surface against the femoral component. A metal-on-metal knee does not exist today, but advances may provide such technology
in the future. The plastic insert helps absorb the impact forces more naturally while allowing reasonable wear for the combined motion. Continuing advances in the manufacture and compostion of the plastic
material have allowed these knees to have expected life of 20-30 years. Most knee replacements use a fixed bearing in which the plastic insert is locked on to its supporting
tibial metal tray, and any rotational movement is accommodated by a slightly loose design at the bearing interface. Fixed bearing design has withstood the test of time as the primary type of knee bearing.
In younger active patients, a mobile bearing design is often a choice. The mobile bearing design allows the plastic material to rotate on its metal tray rather than
being fixed to the tray, potentially allowing more natural knee rotation. Bearing Type: All knee replacements
have a similar bearing material, a hardened polished metal femoral component moving against a plastic polyethylene insert attached to the tibia with a metal supporting tray underneath it. A plastic button
is fixed to the underneath side of the patella to provide an additional bearing surface against the femoral component. A metal-on-metal knee does not exist today, but advances may provide such technology
in the future. The plastic insert helps absorb the impact forces more naturally while allowing reasonable wear for the combined motion. Continuing advances in the manufacture and compostion of the plastic
material have allowed these knees to have expected life of 20-30 years. Most knee replacements use a fixed bearing in which the plastic insert is locked on to its supporting
tibial metal tray, and any rotational movement is accommodated by a slightly loose design at the bearing interface. Fixed bearing design has withstood the test of time as the primary type of knee bearing.
In younger active patients, a mobile bearing design is often a choice. The mobile bearing design allows the plastic material to rotate on its metal tray rather than
being fixed to the tray, potentially allowing more natural knee rotation.
Fixation: The components can be secured to bone by cement or by press-fit. Cement fixation is the standard,
but as technology improves such as porous trabecular metal, press-fit fixation is becoming more common.
Summary
Surgery is not a pleasant prospect for anyone, but for some people with arthritis, it could mean the difference between leading a normal life or putting up with a debilitating condition. Surgery can be regarded as part of your treatment plan-it may help
to restore function to your damaged joints as well as relieve pain.
TKR is one of the most successful operations available today. It is an excellent procedure to improve the quality of life, take away pain and improve function. In general 90-95% of knee replacements survive
15 years, depending on age and activity level.
Surgery is only offered once non-operative treatment has failed. It is an important decision to make and ultimately it is an informed decision between you, your surgeon, family and medical practitioner.
Although most people are extremely happy with their new knee, complications can occur and you must be aware of these prior to making a decision. If you are undecided, it is best to wait until you are sure
this is the procedure for you.
|
|
|